Cardiomyopathy refers to conditions that affect your heart muscle. If you have cardiomyopathy, your heart can’t efficiently pump blood to the rest of your body. As a result, you may experience fatigue, shortness of breath or heart palpitations. Cardiomyopathy gets worse over time. Treatment can slow the progression and improve your quality of life.
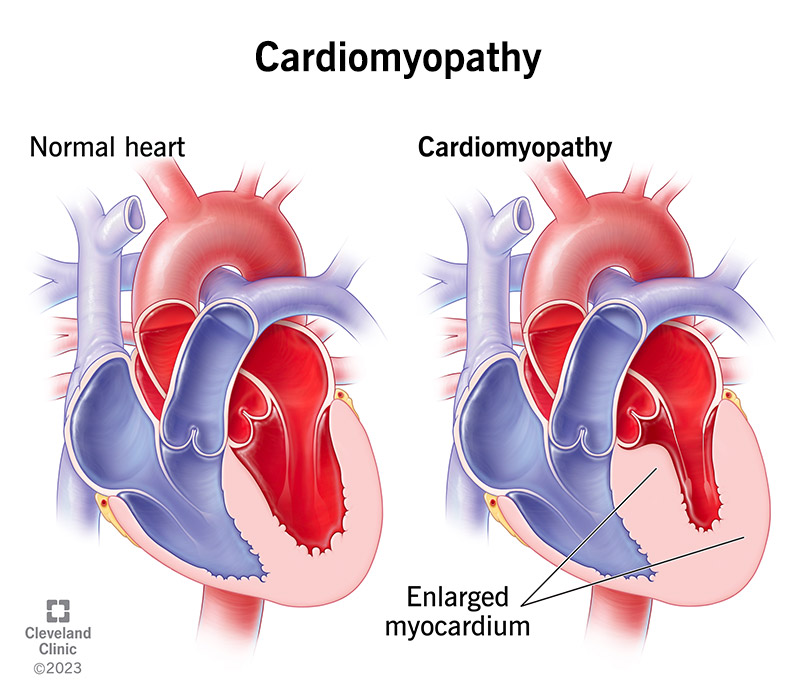
Cardiomyopathy is a disease that affects your myocardium (heart muscle). Cardiomyopathy can make your heart stiffen, enlarge or thicken and can cause scar tissue. As a result, your heart can’t pump blood effectively to the rest of your body.
In time, your heart can weaken and cardiomyopathy can lead to heart failure. Treatment can help. Some people with cardiomyopathy eventually need a heart transplant.
Types of cardiomyopathy include:
Cardiomyopathy can affect anyone of any age, sex or race. The most common inherited cardiomyopathy, hypertrophic, affects about 1 in 500 people in the world. Other genetic types occur in 1 in 2,000 or 2,500 people.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cardiomyopathy symptoms include:
Some people have no symptoms of cardiomyopathy and don’t need treatment. Others experience symptoms as their disease progresses.
Causes of cardiomyopathy include genes you get from your parents. Researchers have found thousands of genetic mutations that cause cardiomyopathies.
Other cardiomyopathy causes include:
Sometimes, experts don’t know the cause of a person’s cardiomyopathy.
Cardiomyopathy risk factors — some of which you can’t change — include:
As cardiomyopathy worsens, you may develop other heart problems, such as:
Your healthcare provider will ask about your medical history and that of your family. They’ll also do a physical exam.
If they suspect you have a heart condition, they’ll refer you to a cardiologist (heart specialist). A cardiologist performs a full assessment that may include a range of diagnostic tests.
Tests to diagnose cardiomyopathy may include:
Cardiomyopathy treatments don’t cure the condition. However, they can help you manage your symptoms and slow down the disease’s progression. Your healthcare provider may recommend lifestyle changes, medications, devices or procedures. They’ll decide your treatment based on which type of cardiomyopathy you have and how advanced it is.
Changing how you live day-to-day can strengthen your heart. Ways to do this include:
Depending on the cause, specific case, your cardiomyopathy and any other underlying medical conditions, certain medications can improve your blood flow and manage your symptoms.
Your cardiologist may prescribe:
Devices a provider puts into your body can treat irregular heart rhythms. These devices monitor your heartbeat. They send electrical impulses to your heart when an arrhythmia starts. You may receive one of these devices:
Some devices help your heart pump blood more efficiently. You may receive one of these devices:
If you have severe symptoms or underlying heart conditions, your provider may recommend a procedure. Some of these involve surgery. Providers usually only recommend open-heart surgery or a heart transplant when all other treatments have failed to bring relief. Most people with cardiomyopathy don’t need the procedures below.
Rarely used procedures may include:
You can take action to reduce your risk of conditions that could lead to cardiomyopathy.
Some of these actions include:
You can’t prevent congenital (inherited) types of cardiomyopathy, but you can let relatives know that you have cardiomyopathy. Your relatives can talk to their providers to see if they’re at risk for it or have it. Early diagnosis helps people make a plan for managing cardiomyopathy.
Cardiomyopathy is a serious condition. Without treatment, it can be life-threatening. It’s also a progressive condition, meaning it usually worsens over time.
Cardiomyopathy treatment can improve your outlook. If you have cardiomyopathy, seek treatment from a cardiologist (heart specialist). Medication, procedures or other treatments can increase your quality of life and help you live longer.
The length of time that you have cardiomyopathy depends on the type you have. The severity of your condition matters, too. Takotsubo cardiomyopathy is usually temporary and doesn’t last long. Cardiomyopathy from alcohol may only last a few months. You may be able to reverse cardiomyopathy from chemotherapy.
For other types, you’ll need to manage your symptoms for the rest of your life. Many people don’t have major problems from their cardiomyopathy, but some do.
There’s no cure for cardiomyopathy. However, you can manage the condition or slow its progression. Many people who make healthy lifestyle choices and seek medical treatment can live a high quality of life with cardiomyopathy. Taking the proper medications can drastically alter and improve the prognosis of cardiomyopathy. Many people can live normal and healthy lives with the right treatment.
Lifestyle choices can affect how quickly cardiomyopathy progresses. To manage symptoms and increase your heart health, your provider may recommend:
You’ll need regular checkups to monitor your heart’s health. Also, you may need regular blood tests or other tests that tell your provider how well your heart is doing. Contact your provider if you have:
Get emergency medical care if you have:
You may want to ask your healthcare provider:
A note from Cleveland Clinic
It’s normal to have concerns about a cardiomyopathy diagnosis. But healthcare providers can offer many treatments to improve your quality of life and help you live longer. Ask your provider how often you need checkups with them. Going to regular appointments with your provider will help them monitor your condition and see how well treatments are working for you.
Last reviewed by a Cleveland Clinic medical professional on 03/14/2023.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy