Uveitis is a condition where you have inflammation of the uvea, which includes the iris, ciliary body and choroid. It’s common, and vision loss is one of the possible complications (especially when uveitis is severe or goes untreated). Fortunately, it’s usually treatable and you can play a big role in improving the odds of a positive outcome.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
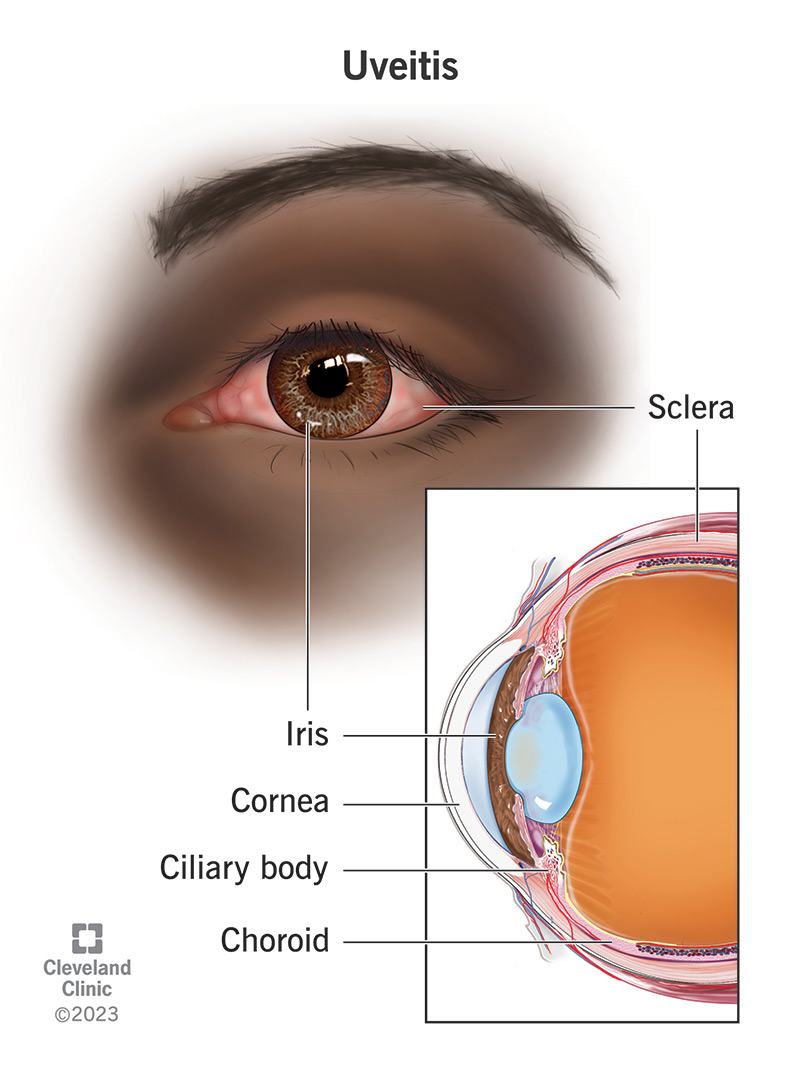
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/14414-uveitis)
Uveitis is inflammation of your uvea, the middle layer of your eye. It can happen for unknown reasons or because of many known conditions. It can affect a specific area of your eye or multiple areas. Depending on the areas it affects, it can be painful, cause redness and irritation, or even disrupt your eyesight. It can affect one eye or both at the same time.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There isn’t a lot of room inside your eyeball for tissue swelling to happen, so it’s easy for swelling to change your eye shape. Your eye shape is a critical part of how you see, and even tiny changes from swelling can disrupt your sight.
In severe cases, uveitis (pronounced “yoo-vee-EYE-tiss”) can cause permanent vision loss and blindness.
Uveitis is common overall. Worldwide, there are about 4 million new cases each year. In the U.S., estimates range from 80,000 to 168,000 cases each year.
Uveitis is more common in adults, and the odds of having it go up with age. It’s less common in children, who make up only 2% to 20% of cases.
The symptoms of uveitis can vary depending on which area of your eye it affects. Experts organize cases into three main areas: anterior, intermediate and posterior. When uveitis affects all three areas, experts call this panuveitis.
The most common of the three is anterior (front) uveitis. It affects the iris and ciliary body, and the symptoms are often visible to you or others. The symptoms of anterior uveitis include:
Advertisement
Intermediate (middle) and posterior (back) uveitis usually cause symptoms that are hard for you or those around you to see. Instead, the symptoms are more likely to affect what you see and/or how well you see it.
The symptoms of intermediate and posterior uveitis include:
Uveitis can happen for many reasons. Between 50% and 70% of cases are idiopathic, meaning the cause isn’t something an eye care specialist can see or test for.
The most likely known causes include:
Infections happen when germs (pathogens) enter your body and cause damage. Infection-related uveitis usually only affects one eye at a time.
Several types of pathogens can cause uveitis, including:
Uveitis isn’t always because of something affecting just your eyes. In some cases, uveitis is a side effect of medications or a symptom of conditions that affect multiple body systems or your whole body (systemic). Systemic causes are more likely to affect both eyes at the same time.
Autoimmune and inflammatory conditions linked to uveitis include:
One specific DNA mutation, HLA-B27, can cause inflammatory arthritis conditions that increase your risk of developing uveitis. These conditions include:
An eye injury can damage the muscles and/or blood vessels that make up different areas of the uvea. When you have an injury, your immune system uses inflammation as part of the repair process. This same process also makes eye surgery a possible cause of uveitis.
But even tiny changes or differences in your eye structure — including those that happen because of inflammation — can be enough to cause uveitis symptoms. The severity of the symptoms depends on many factors, especially the location and severity of the injury.
Advertisement
Certain medications may increase your risk of developing uveitis. These include:
Uveitis isn’t contagious, so you can’t catch it from other people. But it might be a symptom of contagious infections. And some conditions that may cause it can spread from animals to people.
The main complication of uveitis is vision loss and blindness. Complications can happen because of the changes uveitis can cause in your eye. Some of those changes include:
An eye care specialist can diagnose uveitis by asking questions about your symptoms. That includes asking about your medical history and if you’ve had an infection or injury lately. They can also look into your eyes directly or use certain tests to detect signs of uveitis.
Testing for uveitis itself starts with an eye exam, especially parts like the visual acuity test and slit lamp exam. Your specialist may also use tonometry to measure the pressure inside your eye and optical coherence tomography (OCT) to check for changes in the rear structures of your eye.
Advertisement
Other tests are also likely, depending on your symptoms and the suspected causes. Tests your eye care specialist may recommend can include:
Because the tests can vary depending on your symptoms and circumstances, your eye care specialist is the best source of information about specific tests. They can tell you more about these tests and why they recommend them.
Because uveitis can happen for so many reasons, the treatments for uveitis can vary widely. There’s no cure for uveitis, but some conditions that can cause it are curable. When that happens, treating that cause may resolve the uveitis, too.
When there’s no known cause, your eye care specialist may use more general treatments. Treatments can include medications, surgeries and other approaches to help relieve your symptoms and prevent future issues.
Advertisement
Symptom-based treatments usually focus on the following:
Because the treatments can vary so widely, your eye care specialist is the best person to tell you about available options.
What you can expect from uveitis depends on several factors. Some of the most influential factors include:
Because those variables can have such a big impact, your eye care specialist is the best person to tell you what you can expect. They can tailor that information to account for your specific circumstances and case details. They can also advise you on what you can do to help yourself.
Uveitis is a common cause of vision loss and legal blindness. In the U.S., 10% of legal blindness cases happen because of, or in connection with, uveitis. Negative outcomes are more likely when there are delays in diagnosis and treatment. That’s why you shouldn’t ignore it or try to tough it out if you have uveitis symptoms.
The odds of long-term vision issues are much lower with early diagnosis and treatment. When those happen, you’re more likely to recover fully and avoid permanent vision issues.
Unfortunately, uveitis isn’t preventable. Many of its causes happen unpredictably or work in ways experts don’t yet understand. But you can do a few things to reduce your risk of having conditions or events that could lead to uveitis.
The main things you can do are:
If you have uveitis, your eye care specialist will guide you on treatments and tell you what you should do as part of the treatment. Following your eye specialist’s instructions is important because it can reduce your risk of permanent vision loss.
Your eye care specialist will schedule you for follow-up visits, and it’s important to go to them. Those visits help your specialist track your symptoms, the effectiveness of treatments and more.
Your specialist will also tell you about signs and symptoms that mean you need to schedule an appointment or get emergency medical care. Some warning signs that mean you need to call them or get care include:
You may want to ask your healthcare provider:
It can feel scary to have a condition like uveitis and to learn that vision loss is possible. But uveitis is also a condition where you can do a lot to help improve your odds. Early diagnosis and treatment can prevent major issues like permanent vision loss, so you shouldn’t ignore uveitis symptoms.
Once you have a diagnosis, following your eye specialist’s guidance is the best thing you can do to make a good outcome more likely. And if there’s anything you don’t understand about your treatment or what to watch for, your eye care specialist is there to help. Working with them is the best way to help yourself and prevent or minimize future issues.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Uveitis is a serious eye condition that can cause vision loss. At Cleveland Clinic, our experts will create a treatment plan that’s personalized for you.
