What is Coronary Artery Disease?
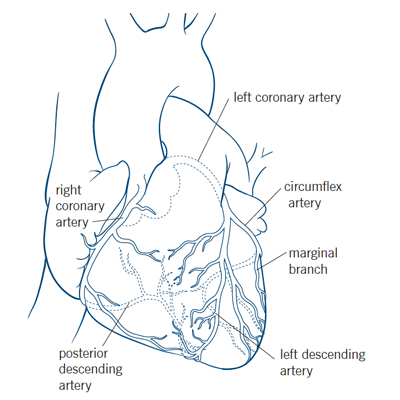
Your heart is a strong muscular pump that is responsible for moving about 3,000 gallons of blood through your body every day. Like other muscles, your heart requires a continuous supply of blood to function properly. Your heart muscle gets the blood it needs to do its job from the coronary arteries.
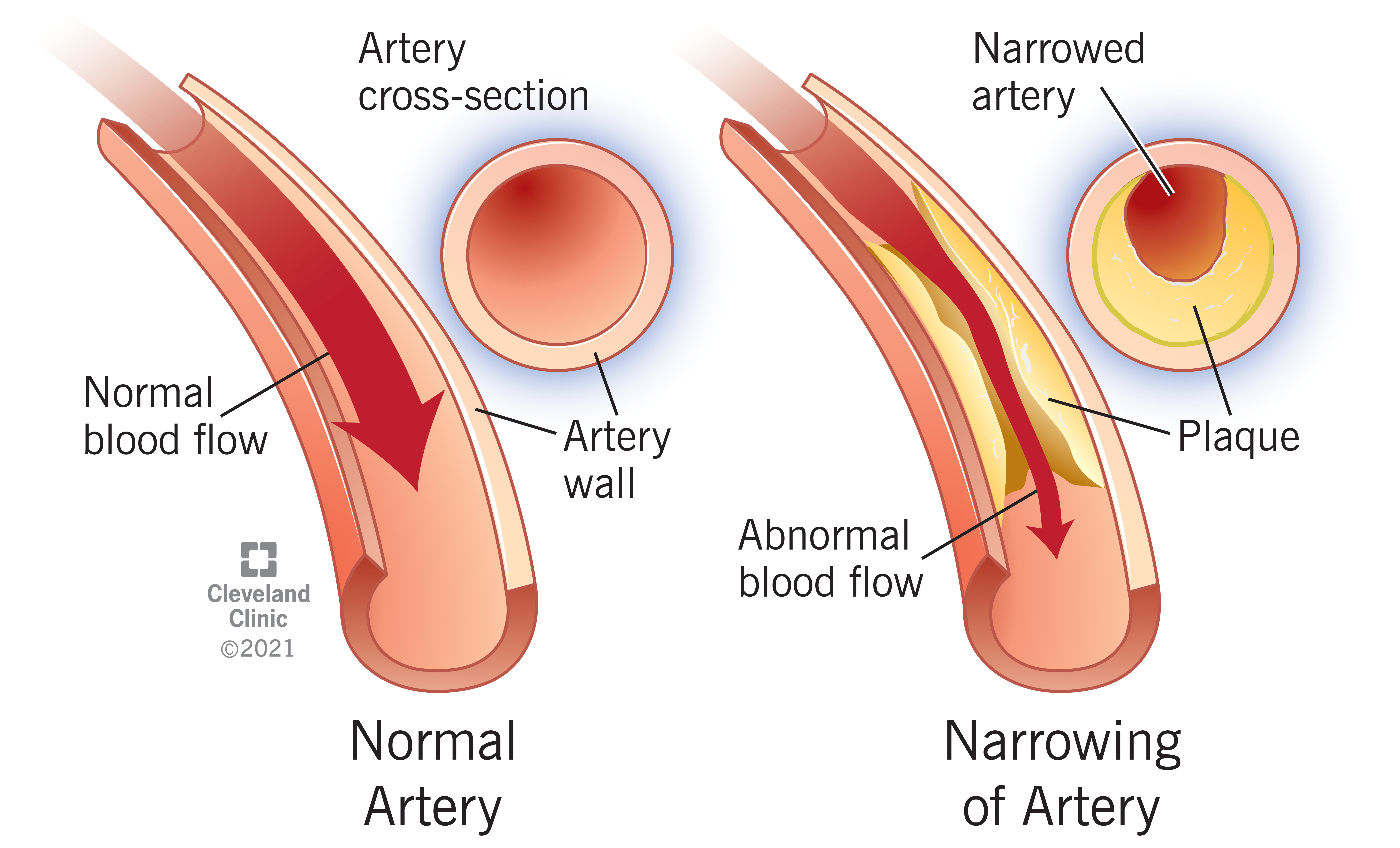
Coronary artery disease is the narrowing or blockage of the coronary arteries, usually caused by atherosclerosis. Atherosclerosis (sometimes called “hardening” or “clogging” of the arteries) is the buildup of cholesterol and fatty deposits (called plaques) on the inner walls of the arteries. These plaques can restrict blood flow to the heart muscle by physically clogging the artery or by causing abnormal artery tone and function.
Without an adequate blood supply, the heart becomes starved of oxygen and the vital nutrients it needs to work properly. This can cause chest pain called angina. If blood supply to a portion of the heart muscle is cut off entirely, or if the energy demands of the heart become much greater than its blood supply, a heart attack (injury to the heart muscle) may occur. Blood flow may also be restricted by narrowing of the small microvessels, which cannot be seen on routine coronary angiography.
Causes
What causes the coronary arteries to narrow?
Your coronary arteries are shaped like hollow tubes through which blood can flow freely. The muscular walls of the coronary arteries are normally smooth and elastic and are lined with a layer of cells called the endothelium. The endothelium provides a physical barrier between the blood stream and the coronary artery walls, while regulating the function of the artery by releasing chemical signals in response to various stimuli.
Coronary artery disease starts when you are very young. Before your teen years, the blood vessel walls begin to show streaks of fat. As you get older, the fat builds up, causing slight injury to your blood vessel walls. Other substances traveling through your blood stream, such as inflammatory cells, cellular waste products, proteins and calcium begin to stick to the vessel walls. The fat and other substances combine to form a material called plaque.
Over time, the inside of the arteries develop plaques of different sizes and types. Plaque that has been present for a long time often calcifies and can become stiff. Newer, or soft plaque, is more likely to progress quickly (but can be reversed by aggressive medical treatment). If the surface of either of these types of plaques tears or becomes eroded, the inner part of the artery becomes exposed to the nearby blood flowing, which leads to blood clots, a worsening of the blockage and sometimes a heart attack (coronary thrombosis.) This spectrum of events is called acute coronary syndromes (see below).
What are acute coronary syndromes?
Unstable angina: This may be a new symptom or a change from stable angina. The angina may occur more frequently, occur more easily at rest, feel more severe, or last longer. Although this can often be relieved with oral medications, it is unstable and may progress to a heart attack. Usually more intense medical treatment or a procedure are required to treat unstable angina.
Non-ST segment elevation myocardial infarction (NSTEMI): This type of heart attack, or MI, does not cause major changes on an electrocardiogram (ECG). However, chemical markers in the blood indicate that damage has occurred to the heart muscle. In NSTEMI, the blockage may be partial or temporary, so the extent of the damage is relatively minimal.
ST segment elevation myocardial infarction (STEMI): This type of heart attack, or MI, is caused by a prolonged period of blocked blood supply. It affects a large area of the heart muscle, and causes changes on the ECG as well as in blood levels of key chemical markers.
Some people have symptoms that indicate they may soon develop an acute coronary syndrome, others may have no symptoms until something happens, and still others have no symptoms of the acute coronary syndrome at all.
All acute coronary syndromes require emergency evaluation and treatment.
Collateral Circulation
As the size of the blockage in a coronary artery increases, the narrowed coronary artery may develop “collateral circulation.” Collateral circulation is the development of new blood vessels that reroute blood flow around the blockage. However, during times of increased exertion or stress, the new arteries may not be able to supply enough oxygenrich blood to the heart muscle.
What is ischemia?
Ischemia is a condition described as “cramping of the heart muscle.” Ischemia occurs when the narrowed coronary artery reaches a point where it cannot supply enough oxygen-rich blood to meet the heart’s needs. The heart muscle becomes “starved” for oxygen.
Ischemia of the heart can be compared to a cramp in the leg. When someone exercises for a very long time, the muscles in the legs cramp up because they’re starved for oxygen and nutrients. Your heart, also a muscle, needs oxygen and nutrients to keep working. If the heart muscle’s blood supply is inadequate to meet its needs, ischemia occurs, and you may feel chest pain or other symptoms.
Ischemia is most likely to occur when the heart demands extra oxygen. This is most common during exertion (activity), eating, excitement or stress, or exposure to cold. When ischemia is relieved in less than 10 minutes with rest or medications, you may be told you have “stable coronary artery disease” or “stable angina.” Coronary artery disease can progress to a point where ischemia occurs even at rest. Ischemia can also occur at rest if a coronary artery suddenly narrows due to a blood clot or arterial spasm.
Ischemia, and even a heart attack, can occur without any warning signs and is called “silent” ischemia. Silent ischemia can occur among all people with heart disease, though it is more common among people with diabetes.
Symptoms
What are the symptoms of coronary artery disease?
The most common symptom of coronary artery disease is angina (also called angina pectoris). Angina is often referred to as chest "pain", but more often it is described as chest discomfort, heaviness, tightness, pressure, aching, burning, numbness, fullness, or squeezing. It can be mistaken for indigestion or heartburn. Angina is usually felt in the chest, but may also be felt in either shoulder, arms, neck, back or jaw.
Other symptoms that may occur with coronary artery disease include:
- Shortness of breath
- Palpitations (irregular heartbeats, skipped beats or a “flip-flop” feeling in your chest)
- A faster heartbeat
- Dizziness
- Nausea
- Extreme weakness
- Sweating
If you experience any of these symptoms, it is important to call your doctor, especially if these are new symptoms or if they have become more frequent or severe.
Symptoms in Women:
Women often have different symptoms of coronary artery disease than men. For example, symptoms of a heart attack in women include:
- Pain or discomfort in the chest, left arm or back
- Unusually rapid heartbeat
- Shortness of breath
- Nausea or fatigue
If any of these symptoms occur, it is important to get medical help right away – call 9-1-1.
What you should do if you have symptoms:
If you or someone you are with has chest, left arm or back pain that lasts more than 5 minutes, with one or more of the symptoms listed previously, call 911 to get emergency help. DO NOT WAIT. Quick treatment of a heart attack is very important to reduce the amount of damage to your heart.
Aspirin: After calling 911, emergency personnel may tell you to chew one full (325 mg) aspirin slowly, if you do not have a history of aspirin allergy or bleeding. Aspirin is especially effective if taken within 30 minutes after the start of symptoms. Do NOT take an aspirin for symptoms of a stroke.
- If your symptoms stop completely in 5 minutes, still call your doctor to report your symptoms.
- Call your doctor if this is the first time you have experienced these symptoms so you can be evaluated.
- Learn to recognize your symptoms and the situations that cause them.
- Call your doctor if you have new symptoms or if they become more frequent or severe.
What’s the difference between angina and a heart attack?
Angina is a warning symptom of heart disease – but it is not a heart attack. The symptoms of a heart attack (also called myocardial infarction or “MI”) are similar to angina.
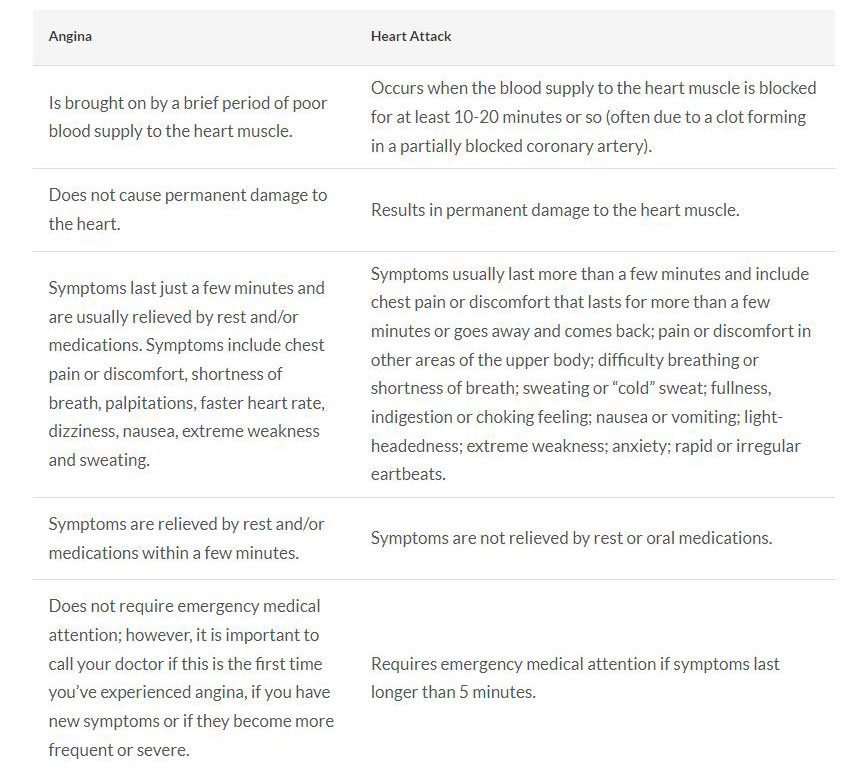
If you have been prescribed nitroglycerin and experience angina: Stop what you are doing and rest. Take one nitroglycerin tablet and let it dissolve under your tongue, or if using the spray form, spray it under your tongue. Wait 5 minutes. If you still have angina after 5 minutes, call 911 to get emergency help.
For patients diagnosed with chronic stable Angina: If you experience angina, take one nitroglycerin tablet and let it dissolve under your tongue, repeating every 5 minutes for up to 3 tablets spanning 15 minutes. If you still have angina after taking 3 doses of nitroglycerin, call 911 to get emergency help.
Reference: 2012 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction (Updating the 2007 Guideline and Replacing the 2011 Focused Update)
Use of aspirin with unstable chest pain: After calling 911, emergency personnel may tell you to chew one full aspirin (325 mg) slowly, if you do not have a history of aspirin allergy or bleeding. Aspirin is especially effective if taken within 30 minutes after the start of symptoms. Do NOT take an aspirin for symptoms of stroke. Continue to take your nitroglycerin as prescribed.
Do not wait to get help
At the first signs of a heart attack, call for emergency treatment (911). Do not wait for your symptoms to “go away.” Early recognition and treatment of heart attack symptoms can reduce the risk of heart damage and allow treatment to start immediately. Even if you’re not sure your symptoms are those of a heart attack, you should still be evaluated.
Diagnosis
How is coronary artery disease diagnosed?
Your doctor diagnoses coronary artery disease by talking to you about your symptoms, reviewing your medical history and risk factors, and performing a physical exam.
Diagnostic tests, including blood tests, an electrocardiogram (ECG or EKG), exercise or pharmacologic stress tests, coronary computed tomography angiogram (CTA), or cardiac catheterization may be required to appropriately diagnose and treat coronary artery disease. These tests help your doctor evaluate the extent of your coronary heart disease, its effect on the function of your heart, and the best form of treatment for you. n order to diagnose certain conditions like microvascular coronary disease or spasm, your doctor may recommend more specialized tests.
Risks
What are the risk factors for coronary artery disease?
Non-modifiable risk factors (those that cannot be changed) include:
- Male sex. The risk of heart attack is greater in men than in women, and men have heart attacks earlier in life than women. However, at age 70 and beyond, men and women are equally at risk.
- Advanced age. Coronary artery disease is more likely to occur as you get older, especially after age 65.
- Family history of heart disease. If your parents have heart disease (especially if they were diagnosed with heart disease before age 50), you have an increased risk of developing it. Ask your doctor when it’s appropriate for you to start screenings for heart disease so it can be detected and treated early.
- Race. People who are Black have more severe high blood pressure than people who are White and therefore have a higher risk of heart disease. Heart disease risk is also higher among Americans of East Asian descent, Mexican Americans, American Indians and native Hawaiians. This is partly due to higher rates of obesity and diabetes in these populations.
- Chronic kidney disease.
- Pre-eclampsia or gestational diabetes.
Modifiable risk factors (those you can treat or control) include:
- Cigarette smoking and exposure to tobacco smoke.
- High blood cholesterol and high triglycerides – especially high LDL or “bad” cholesterol over 100 mg/dL and low HDL or “good” cholesterol under 40 mg/dL. Some patients who have existing heart or blood vessel disease and other patients who have a very high risk should aim for a LDL level less than 55-70 mg/dL. Your doctor can provide specific guidelines.
- High blood pressure (130/80 mm/Hg or higher).
- Poorly managed diabetes. (having an A1C greater than 8% for a year or more despite standard care).
- Having overweight (body mass index or BMI from 25-29 kg/m2) or obesity (BMI higher than 30 kg/m2).
NOTE: How your weight is distributed is important. Your waist measurement is one way to determine fat distribution. Your waist circumference is the measurement of your waist, just above your navel. The risk of cardiovascular disease increases with a waist measurement of over 35 inches in women and over 40 inches in men. - Untreated sleep apnea.
- Poorly managed stress or anger.
- Diet high in saturated fat and cholesterol.
- Drinking too much alcohol.
- Poorly managed autoimmune conditions such as lupus or rheumatoid arthritis.
The more risk factors you have, the greater your risk of developing coronary artery disease.
Treatments
How is coronary artery disease treated?
Treatment for coronary artery disease involves reducing your risk factors, taking medications as prescribed, possibly undergoing invasive and/or surgical procedures and seeing your doctor for regular visits. Treating coronary artery disease is important to reduce your risk of a heart attack or stroke.
Reduce your risk factors
Reducing your risk factors involves making lifestyle changes. Your doctor will work with you to help you make these changes.
- If you smoke, you should quit.
- Make changes in your diet to reduce your cholesterol, manage your blood pressure, and manage blood sugar if you have diabetes. Low-fat, low-sodium and low-cholesterol foods are recommended. Limiting alcohol to no more than one drink a day is also important. Registered dietitians can help you make the right dietary changes. Cleveland Clinic offers nutrition programs and classes to help you reach your goals.
- Increase your exercise/activity level to help achieve and maintain a weight that's healthy for you and reduce stress. Generally, at least 150 minutes per week of exercise is recommended. At least 75 minutes of vigorous cardiac activity (defined as at least a brisk walk) combined with 20-40 minutes of light weight lifting is advised per week. But, check with your doctor before starting an exercise program. Ask your doctor about participating in a cardiac rehabilitation program.
Take medications as prescribed
If lifestyle changes aren’t enough to control your heart disease, medications may be prescribed to treat certain risk factors, such as high cholesterol or high blood pressure. The medications prescribed will depend on your personal needs, presence of other health conditions and your specific heart condition.
In general, lifestyle changes and medications are the best ways to reduce the risk of a heart attack. In some instances, stenting or bypass surgery provide additional benefit. Importantly, they are usually effective at reducing the symptoms of coronary artery disease.
Have procedures to treat coronary artery disease, as recommended
Interventional procedures
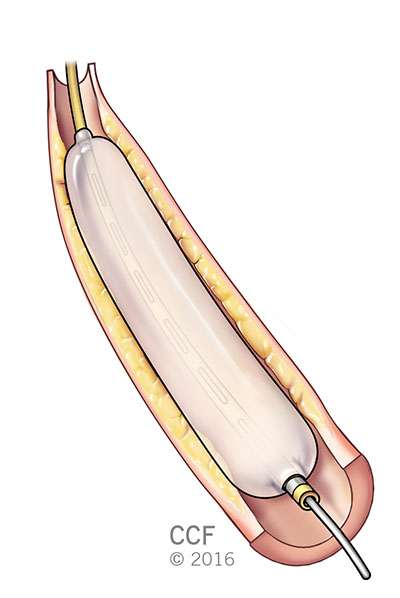
The most common interventional treatment of a blocked artery is placement of a coronary stent in a cath lab. Expansion of the stent should be verified by use of intravascular ultrasound or optical coherence tomography. Current stents are all coated with a medicine designed to prevent scar tissue formation that can sometimes lead to later stent narrowing. These procedures are considered non-surgical because they are done by a cardiologist through a tube or catheter inserted into a blood vessel, rather than by a surgeon through an incision. The physician chooses the type of procedure based on individual patient needs.
Coronary artery bypass graft (CABG) surgery
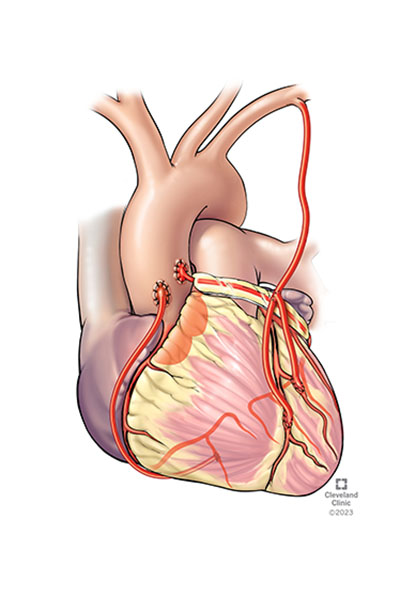
One or more blocked coronary arteries are bypassed by a blood vessel graft to restore normal blood flow to the heart. These grafts usually come from the patient’s own arteries and veins located in the chest, arm or leg. The graft goes around the clogged artery (or arteries) to create new pathways for oxygen-rich blood to flow to the heart.
Coronary artery bypass graft (CABG), also known as bypass surgery, usually achieves the most durable (long-lasting) outcomes and can improve survival in patients with complex coronary artery disease. During a traditional CABG surgery, a cardiothoracic surgeon will make an incision in the center of your chest to reach your heart. They’ll also split your breastbone (sternum) down the middle, then spread and lift your rib cage to make it easier to access your heart. A heart-lung machine takes over pumping blood through your body during the surgery. However less invasive approaches are possible in select patients. Less invasive options may use smaller incisions or might not include opening the sternum.
When these traditional treatments are not options for you, doctors may suggest other less traditional therapies, including EECP.
Enhanced external counterpulsation (EECP)
For patients who have persistent angina symptoms and have exhausted the standard treatments without successful results, EECP may stimulate the openings or formation of collaterals (small branches of blood vessels) to create a natural bypass around narrowed or blocked arteries. EECP is a non-invasive treatment for people who have chronic, stable angina; who are not receiving adequate relief from angina by taking nitrate medications; and who do not qualify for a procedure such as bypass surgery, angioplasty or stenting.
Important Note: These procedures increase blood supply to your heart, but they do not cure coronary heart disease. You will still need to decrease your risk factors by making lifestyle changes, taking medications as prescribed and following your doctor’s recommendations to reduce the risk of future disease development.
Follow-Up Care
Your cardiologist (heart doctor) will want to see you on a regular basis for a physical exam and possibly to perform diagnostic tests. Your doctor will use the information gained from these visits to monitor the progress of your treatment. Check with your heart doctor to find out when to schedule your next appointment.
Who is affected by coronary artery disease?
Heart disease is the leading cause of death in the United States in men and women. Coronary artery disease affects 20.5 million Americans. The American Heart Association (AHA) estimates that about every 40 seconds, an American will have a heart attack.
Appointments
To make an appointment or to learn more about coronary artery disease and available treatment options, please contact the heart, vascular & thoracic resource center nurse toll-free at 866.289.6911.
For More Information
For more information about coronary artery disease and treatments, please visit our website at www.clevelandclinic.org/heart or e-mail us using the Contact Us form. We would be happy to answer your questions.
Virtual Second Opinion
Cleveland Clinic's Virtual Second Opinion program connects patients to the expertise of top Cleveland Clinic specialists without the time and expense of travel. Through our secure web platform, patients can submit their detailed health information, medical records and diagnostic test results. The most appropriate Cleveland Clinic expert is assigned to the consultation and will render a detailed second opinion. The report includes commentary about the diagnosis and treatment options or alternatives and recommendations regarding future therapeutic considerations. Patients are also able to send additional questions to the physician who provided the report. Online medical second opinions are available for more than 1,200 medical diagnoses.
Talk to a Heart Nurse
For over 15 years Heart, Vascular & Thoracic resource nurses have been offering assistance to people who have questions or concerns about heart and vascular conditions. Nurses are available to help with questions on symptoms, diagnoses, treatment options, Cleveland Clinic services and doctors, etc. The nurses are available weekdays from 8:30 a.m. – 4 p.m., Eastern Time, through phone or email. If you need help, you may contact a nurse.
Why Choose Us?
Coronary Artery Disease Center
The Coronary Artery Disease Center brings a multi-disciplinary approach to the diagnosis and treatment of patients who have severe ischemic coronary heart disease and for whom the therapeutic options locally are limited. The center consists of specialists from interventional cardiology, cardiothoracic surgery, cardiac imaging, electrophysiology, prevention and nutrition, pain management, stem cell therapy, pharmacy and nursing. We provide:
- A thorough evaluation of patients using state-of-the-art diagnostic testing.
- Multi-disciplinary approach to comprehensive care for patients with advanced ischemic diseases.
- Ongoing research and education to provide patients with high-quality and innovative therapies.
About the Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute
The Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute at Cleveland Clinic is one of the largest cardiovascular specialty groups in the world, providing patients with expert medical management and a full range of therapies. Cleveland Clinic’s Heart, Vascular & Thoracic Institute is nationally and internationally renowned for the world’s best cardiovascular care.
Our areas of expertise combine research, education and clinical practice to provide innovative and scientifically based treatments for cardiovascular disease. The commitment of our physicians and scientists to the prevention and cure of cardiovascular disease has led to innovative care, better outcomes and improved quality of life for patients with cardiovascular disease.
This information is not intended to replace the medical advice of your doctor or health care provider.
Please consult your health care provider for advice about a specific medical condition.
Resources
Learn More
- Learn more about coronary artery disease by visiting Cleveland Clinic’s Heart, Vascular & Thoracic Institute website
- Watch videos on coronary artery disease presented by Cleveland Clinic specialists
- Sign up for our e-newsletter, and get tips on maintaining a heart healthy lifestyle, recipes and essential health news
- Listen to podcasts from our Cleveland Clinic Heart, Vascular & Thoracic physicians.