Types of Pain
Types of Hip Pain
Chronic hip pain can change your life by limiting your ability to walk, sit comfortably or perform normal daily activities. When hip pain interferes with your ability to do the things you want or need to do each day, it is time to seek medical advice.
What are the different types of hip pain?
Hip pain has many causes. Some of the most common conditions causing hip pain include:
Osteoarthritis
Osteoarthritis is a wearing down of the cartilage that allows the bones to glide smoothly over one another in joints such as the hip. It is one of the most common causes of hip pain in people over 65. As the cartilage wears away, the head of the thigh bone rubs directly against the inner hip socket. Splinters of bone and cartilage can interfere with normal hip movement.
Pain in the groin and front of the thigh is the most common symptom of hip arthritis, especially when walking or during activities that require twisting, such as putting on socks or getting out of a car. The pain is caused by the bones rubbing against each other. The hip joint also may become swollen and stiff.
Hip fractures
Older individuals are susceptible to breaking a hip during normal everyday activities if their bones are weak due to osteoporosis. Although osteoporosis chiefly affects women, men over 65 are at risk as well. Hip fractures are medical emergencies and typically require immediate surgery.
In addition, younger active individuals can develop stress fractures of the hip. When muscles become fatigued, they fail to absorb the shock of impact from jumping and other activities, and forces are transferred to the bone itself, causing tiny cracks. Stress fractures in the hip joint can cause pain.
Bursitis
Bursitis is inflammation of any of the fluid-filled sacs protecting the body’s joints after an injury or due to overuse. Trochanteric bursitis affects the outer surface of the hip joint, producing pain when lying on the affected side, standing up, walking, climbing steps or driving. Treatment typically consists of anti-inflammatories, physical therapy (including stretching and muscle strengthening) and injections.
Osteonecrosis
Insufficient blood flow to bone can destroy bone cells, a process called osteonecrosis (also avascular or aseptic necrosis). There are many causes of this condition, but it is commonly caused by corticosteroid use for different medical conditions. Smoking can also cause the condition. The hip is the most common site affected by osteonecrosis. Treatment options are many and diverse. Early consultation with a hip expert is recommended.
Tendonitis
The tendons – rope-like connective tissues connecting muscles to bone at the hip and other joints – can become painfully inflamed by repetitive and strenuous movement. Tendonitis is a common sports injury, caused by overuse of the same parts of the body.
Strains
Strains are small tears in the muscle from overuse/irritation. Lower back strains can be caused by twisting, quickly turning, and “pulling” the muscles that support the spinal column. The back and hip muscles often become strained because the abdominal muscles are too weak to lend support.
Herniated discs
Falls and heavy lifting can injure the discs, the “shock absorbers” in the spinal column. They separate and cushion the vertebrae, but as we age the discs become more brittle and can rupture, or herniate. Pain from a ruptured disc in the lower spine can radiate down the nerve extending from the spinal cord to the leg (sciatica). This type of pain is differentiated from hip osteoarthritis in that it is typically felt in the lower back and buttock region, radiating down the leg, whereas hip arthritis pain is felt in the groin occasionally radiating down to the knee.
Septic hip
Septic arthritis is an infection of the hip joint, which develops most commonly in young children and older adults. Bacteria enter the bloodstream and settle in the hip, resulting in pain and limping. Fever, and warmth and redness over the hip, point to possible infection – requiring urgent treatment ranging from antibiotics to operative intervention.
Labral tears
The hip labrum is an “O-ring” of fibrocartilage that lines the edge of the socket portion of the hip (ball and socket) joint. The labrum may become injured, torn and painful due an accident, sports injury or, more commonly, occur over time when the ball portion of the joint rubs abnormally against the socket or doesn’t have the full range of motion. Treatment may include non-steroidal anti-inflammatories, physical therapy and activity modification/rest. If this fails, corticosteroid injections or surgery may be needed.
Diagnosis

How is hip pain diagnosed?
If you develop hip pain that persists, physicians in Cleveland Clinic’s Orthopaedic & Rheumatologic Institute can help sort out the possible causes.
When diagnosing any hip pain, the physician will take your medical history and perform a thorough physical examination. To help your doctor best understand your hip pain, you’ll need to provide the following information:
- A description of your hip pain (aching, tenderness, burning, or swelling)
- Where the pain is located and when it occurs
- When the pain started (and if it is the result of an injury or accident)
- Anything that makes the pain worse or better
Your doctor also may order imaging tests to view the joint, which may include the following:
- X-rays.
- MRI.
If an X-ray looks normal, your doctors may order a magnetic resonance imaging (MRI) scan. A MRI provides more detail about your soft tissues and cartilage than an X-ray.
Non-Surgical Treatments
Non-surgical Treatments
How is hip pain treated?
Many types of hip pain can be resolved with conservative treatments such as:
Rest – When the hip is inflamed, as in bursitis, tendonitis or arthritis, it is important to rest the joint and avoid overusing it.
Ice – Applying cold packs or ice bags to the hip when pain is severe can reduce inflammation and swelling.
Physical Therapy – Once your doctor diagnoses the cause of your hip pain, physical therapists can show you stretches and exercises to increase flexibility and strength in the hip. Physical therapists can also advise you about helpful aerobic exercises, such as swimming, aqua therapy or cycling, which may not aggravate hip pain as high-impact activities would. You may be advised to lose weight to relieve pressure on your joints. For problems such as bursitis, they can use ultrasound and massage techniques. Finally, physical therapists will show you good “body mechanics” – the proper ways to sit, stand, lift and sleep – to avoid aggravating hip pain.
Pain Relievers – Anti-inflammatory medicines can be purchased over the counter to relieve hip pain if needed, and include ibuprofen (Advil®) or naproxen (Aleve®).
Injections – For hip problems caused by inflammation, steroids may be injected to settle the inflammation down. Injection for trochanteric bursitis is easily provided in the physician’s office, but deep hip joint infections may need image guidance (ultrasound or x-rays) to help localize the injection.
Surgical Treatments
Surgical Treatments
Hip problems such as osteoarthritis do not disappear on their own. They tend to worsen with age, and eventually conservative measures may not be enough to control pain. At that point, your doctor may recommend surgery.
Hip arthroscopy
Arthroscopy is a minimally invasive surgical procedure used to diagnose and treat hip problems that do not respond to nonsurgical treatment, such as a labral (cartilage) tear, tendon release or bursitis. It is done using an instrument called an arthroscope.
The arthroscope has a light source and a camera. During hip arthroscopy, the surgeon shines a light into the joint, and with the help of the camera, an image of the hip joint is then viewed on a TV monitor. By seeing the hip joint through the arthroscope, the surgeon does not need to make a large incision. Sterile fluid is used to expand the joint, which increases visibility in the joint area and makes it easier for the surgeon to work.
The surgery is performed under a general local anesthetic and pain medications are administered after the procedure for pain control. Two to five small incisions (approximately half an inch long) are made on the side of the hip.
An arthroscope is inserted, and the surgeon looks inside the hip. Other instruments may be used during surgery to cut, shave, remove particles in the joint, or repair tissue. Local anesthetic and pain medication are administered into the joint after the procedure for pain control. Arthroscopy can help relieve pain due to many problems that can cause damage to the joint, particularly labral tears.
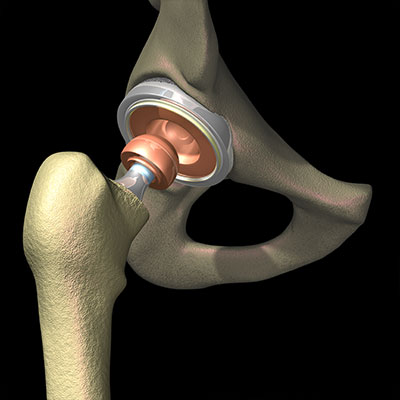
Hip replacement
In severe osteoarthritis, hip pain can become constant, and joint swelling and stiffness can cause limping and difficulty moving. This may cause individuals to restrict their normal daily activities. In these cases, hip replacement surgery can dramatically improve the quality of life. Today, more than 200,000 total hip replacements are performed each year in the United States, with this number projected to rapidly increase over the next decade. Besides osteoarthritis, hip replacement may be indicated for hip fractures, bone tumors that break down the hip, and osteonecrosis – if the disease has gone untreated for a long time and has progressed to a point where the joint cannot be saved.
During the procedure, the orthopaedic surgeon removes damaged cartilage and bone from the hip socket, as well as the ball and upper end of the thigh bone (femur). An artificial joint, or prosthesis, made of a combination of metal and plastic or ceramic, replaces the hip socket, and the head and upper end of the femur. The prosthesis parts must sometimes be cemented in place. Your surgeon will determine what type of implant is the most appropriate for you.
Recovery – Physical therapy is key to recovering mobility and can begin the day of surgery in some cases. Helping patients get out of bed and put weight on the new hip can help speed recovery. Recovery is individualized, but in general, the younger you are, the faster your rehabilitation and recovery are likely to be, and the less time you’ll spend in the hospital. Many patients can walk normally, without a cane, four to six weeks after surgery.
After completing rehabilitation, most patients can perform daily activities easily and without pain. They can return to recreational pastimes such as walking, cycling, golf, skiing, and tennis. Patients may be able to run or jog after a hip replacement depending on their pre-surgical conditioning, but jumping from heights is not recommended.
Benefits – A hip replacement will help debilitating pain that is unrelieved by conservative approaches, such as rest or pain relievers. The procedure helps restore range of motion and return patients to their daily activities.
Who is a candidate? – Your orthopaedic surgeon will determine if you are a candidate based on your level of pain, disability and overall health.
Risks – The risk for complications after hip replacement surgery is low. Fewer than 2 percent of patients experience serious complications (for example, joint infection). Having a chronic health condition may increase your risk for complications that may prolong or limit your recovery. In particular, obesity, diabetes, smoking, and kidney failure pose the highest risk for complications.
- Infection and dislocation are the most serious device-related complications; luckily they remain rare with approximately 1% incidence.
- Inaccurate leg length may occur or become more noticeable after surgery, but this perception typically improves after 3 months.
- Blood clots in the leg is a possible complication after hip replacement, particularly in patients who are not ambulating well. Your orthopaedic surgeon may prescribe blood thinners to prevent them.
- Some patients also experience complications, including dislocation, nerve and blood vessel injury, bleeding, fracture, stiffness or pain.
Durability – Hip replacement surgery has been performed all over the world for more than three decades, with many refinements in the operation and in the design of hip prostheses during this time. With newer materials, loosening or wearing out is now less common. Today’s artificial hips can last up to 30 years, important for middle-aged individuals facing hip replacement.
Robotic Surgery
Robotic-assisted surgery is an emerging technology that assists surgeons in fine tuning joint replacement surgery. At Cleveland Clinic Florida, orthopaedic surgeons now perform joint replacement surgery using robotic-assisted technology in many patients. Surgical robots can add accuracy and precision to total joint replacement surgery. If you're planning for a total hip replacement surgery, talk with your orthopaedic surgeon to determine if you may be a candidate for robotic-assisted surgery.
Hip Resurfacing
Hip Resurfacing
For some younger, active patients with hip pain due to arthritis, injury or hip osteonecrosis, hip resurfacing is an alternative to total hip replacement. It offers long-lasting pain relief and a return to normal activities.
Approved in 2006 by the U.S. Food and Drug Administration (FDA), hip resurfacing involves shaving away a few millimeters of bone in the hip joint, instead of removing several inches of the upper thigh bone. Then the joint surfaces are capped with a metal implant. Hip resurfacing preserves more bone than hip replacement and allows for easy hip replacement down the road, if needed.
Recovery – Patients can expect to be on crutches for six weeks after hip resurfacing surgery. Physical therapy begins in the hospital and most patients learn all the exercises they need to do before they go home. In the first months of recovery, activities gradually increase, and in about one year, patients will be able to resume all their routine activities without any restrictions, including running, jumping, sports, and demanding occupations.
Benefits – The advantages include keeping more of your own bone, which feels more natural. Normal loading of the bone is maintained, which supports bone health. Unequal leg lengths and dislocation (“popping out”) are both much less common than with total hip replacement. Most importantly, hip resurfacing offers unrestricted activity. Even professional athletes have returned to competition after resurfacing. And, in the unusual situation where additional surgery is needed, patients who have hip resurfacing have better options.
Candidates – Hip resurfacing is not for everyone. Candidates are active people under age 65, and are generally men in good health. Many are looking for an alternative to hip replacement that does not result in lifelong activity restrictions. It is also an option for young patients who have been advised to delay having total hip replacement, which achieves better results in older individuals. Women are not the best candidates and would be considered only in special circumstances. Because most doctors do not perform hip resurfacing, this option is often not considered.
Risks – There are two main risks involved in hip resurfacing. In less than 1% of cases, patients who undergo the procedure subsequently suffer a fracture of the femoral neck, where the implant was placed. If this occurs, it usually happens within six months of a resurfacing operation, in which case the patient will likely transition to total joint replacement. But the good news is that the hip socket doesn’t have to be changed, and a standard implant will be used rather than a long, revision-style device. At Cleveland Clinic, the risk of fracture is about 0.1%.
The other potential risk is related to the metals – cobalt and chromium – that comprise the components of a resurfaced joint. Tiny amounts of these metals can be detected in the bloodstream after hip resurfacing. There is no indication of health problems at these very low levels, and over time the levels may return to normal. Only in rare cases, higher than expected metal levels may necessitate further surgery. That is why candidates are required to have normal kidney function, needed to keep metal levels low. In addition, patients who have undergone resurfacing have been found to have a lower risk of cancer in the future and greater life expectancy compared to those receiving traditional total hip replacement.
Durability – Metal-on-metal hip resurfacing has been performed for many years. The device currently in use was developed in 1997 and approved in the U.S. in 2006. From long-term data, we know that men are the best candidates. At Cleveland Clinic, the 10-year success rate in men is 99%, with an average age of 53. The 20-year success rate in men from centers in other countries is 98%. These results exceed those for total hip replacement in young, active individuals.
Patient Services
MyChart
MyChart is a secure online tool that provides personalized health information from the privacy of your home at any time, day or night. Learn more or login now.
Appointments
Making an appointment
Call 877.463.2010 for Weston & Indian River and 844.630.4968 for Martin Health or visit us online to make an appointment with a hip pain specialist with Cleveland Clinic Florida’s Orthopaedic & Rheumatologic Institute. Visit us online to learn more about the Hip & Knee Surgery program at Cleveland Clinic Florida.
Why Choose Us?
Why should I choose Cleveland Clinic Florida?
The Orthopaedic & Rheumatologic Institute at Cleveland Clinic Florida specializes in treating individuals affected by bone, joint or connective tissue disorders. Our team of physicians, physician assistants, nurses and specialized support staff at Cleveland Clinic Weston Hospital, Cleveland Clinic Indian River Hospital and Cleveland Clinic Martin Health Hospitals provide world-class care and offer extensive expertise in orthopaedic, sports medicine and rheumatology specialties.
The physicians and surgeons at Cleveland Clinic Florida’s Orthopaedic & Rheumatologic Institute are recognized as among the best in the world for hip assessment and repair. We use a multidisciplinary team approach, with all of the experts you need under one roof, including orthopaedic physicians and surgeons, rheumatologists and physical therapists.
With a broad range of treatment options, state-of-the-art diagnostics and decades of experience, we can evaluate the cause of your shoulder pain and determine the treatment that is best for you. Cleveland Clinic Florida’s orthopaedic program has a consistent history of excellence and innovation, and has been rated as high-performing by U.S. News & World Report.
