Colon cancer develops from polyps (growths) in your colon’s inner lining. Healthcare providers have screening tests and treatments that detect and remove precancerous polyps. If untreated, colon cancer may spread to other areas of your body. Thanks to these tests, early treatment and new kinds of treatment, fewer people are dying from colon cancer.
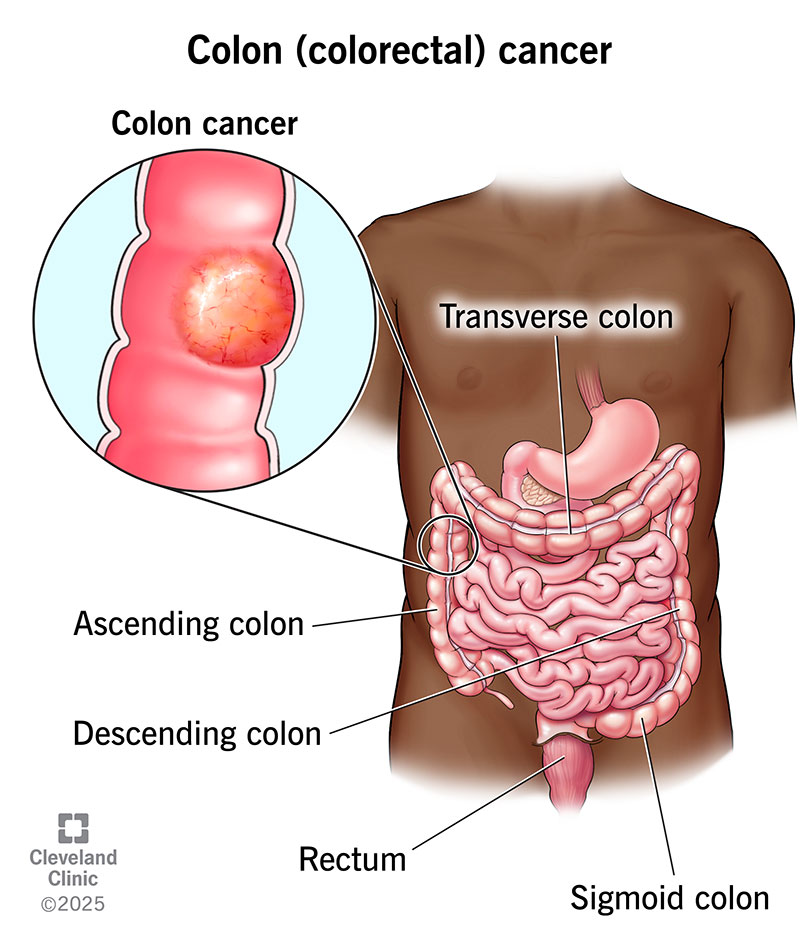
Colon (colorectal) cancer starts in your colon (large intestine), the long tube that helps carry digested food to your rectum and out of your body.
Colon cancer develops from certain polyps or growths in the inner lining of your colon. Healthcare providers have screening tests that detect precancerous polyps before they can become cancerous tumors. Colon cancer that’s not detected or treated may spread to other areas of your body. Thanks to screening tests, early treatment and new kinds of treatment, fewer people are dying from colon cancer.
Your colon wall is made of layers of mucous membrane, tissue and muscle. Colon cancer starts in your mucosa, the innermost lining of your colon. It consists of cells that make and release mucus and other fluids. If these cells mutate or change, they may create a colon polyp.
Over time, colon polyps may become cancerous. (It usually takes about 10 years for cancer to form in a colon polyp.) Left undetected and/or untreated, the cancer works its way through a layer of tissue, muscle and the outer layer of your colon. The colon cancer may also spread to other parts of your body via your lymph nodes or your blood vessels.
Colon cancer is the third most common cancer diagnosed in people in the U.S. According to the U.S. Centers for Disease Control and Prevention (CDC), men and people assigned male at birth (AMAB) are slightly more likely to develop colon cancer than women and people assigned female at birth (AFAB). Colon cancer affects more people who are Black than people who are members of other ethnic groups or races.
Colon cancer typically affects people age 50 and older. Over the past 15 years, however, the number of people age 20 to 49 with colon cancer has increased by about 1.5% each year. Medical researchers aren’t sure why this is happening.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You can have colon cancer without having symptoms. If you do have symptoms, you may not be sure if changes in your body are signs of colon cancer. That’s because some colon cancer symptoms are similar to symptoms of less serious conditions. Common symptoms of colon cancer include:
Like all types of cancer, colon cancer happens when cells grow and divide uncontrollably. All cells in your body are constantly growing, dividing and dying. That’s how your body remains healthy and working as it should. In colon cancer, cells lining your colon and rectum keep growing and dividing even when they’re supposed to die. These cancerous cells may come from polyps in your colon.
Medical researchers aren’t sure why some people develop precancerous colon polyps that become colon cancer. They do know certain risk factors increase people’s chances of developing precancerous polyps and colon cancer.
Those risk factors include certain medical conditions, including inherited conditions, and lifestyle choices. Having one or more risk factors for colon cancer doesn’t mean you’ll develop the condition. It just means you have increased risk. Understanding risk factors may help you decide if you should talk to a healthcare provider about your risk of developing colon (colorectal) cancer.
Healthcare providers use several tests to diagnose colon cancer. Those tests include:
A cancer screening test checks for cancer when you don’t have any signs or symptoms of cancer. If your screening test shows abnormalities, a healthcare provider may recommend additional tests.
A colonoscopy is the most common screening test for colon cancer. Other tests include:
Healthcare providers use the TNM cancer staging system developed by the American Joint Committee on Cancer to stage colon cancer.
There are five stages of colon cancer. Three of the four stages have three sub-stages. The colon cancer staging system includes the following:
Stage 0: Healthcare providers may refer to this as carcinoma in situ. When they do, they’re talking about abnormal or precancerous cells in your mucosa, the innermost layer of your colon wall.
Stage I: Stage I colorectal cancer has grown into the wall of your intestine but hasn’t spread beyond the muscular coat or into close lymph nodes.
Stage II: The cancer has spread farther into the wall of your intestine but hasn’t spread to nearby lymph nodes. There are three types of Stage II colon cancer:
Stage III: In this stage, colon cancer has spread to your lymph nodes. Like Stage II colon cancer, there are three sub-stages of Stage III colon cancer:
Stage IV: Cancer has spread (metastasized) to other areas of your body, such as your liver, lungs or ovaries:
Surgery is the most common colon cancer treatment. There are different colon cancer surgeries and procedures:
Healthcare providers may combine surgery with adjuvant therapy. This is cancer treatment done before or after surgery. They may also use these treatments for colon cancer that has spread or come back. Treatments may include:
You may not be able to prevent colon cancer, but you can reduce your risk of developing the condition by managing risk factors:
According to U.S. National Cancer Institute (NCI) data, more than 90% of people treated for early-stage colorectal cancer were alive five years after diagnosis. (NCI data doesn’t break out separate survival rates for colon and rectal cancer.)
NCI data shows that overall, 65% of people with colorectal cancer were alive five years after diagnosis. (A survival rate is an estimate based on the experiences of people with specific kinds of cancer.)
Colorectal cancer survival rates vary based on the cancer stage at diagnosis. For example, 73% of people with colorectal cancer that’s spread to nearby tissues, organs or lymph nodes were alive five years after diagnosis. That five-year survival rate drops to 17% if the cancer spreads to a distant organ or lymph node.
A survival rate is an estimate based on outcomes — how long people lived after treatment for a specific type of cancer. In this case, survival rates are based on the experiences of large groups of people who have colorectal cancer, and not just colon cancer. In addition, many things affect colon cancer survival rates. If you have this condition, your healthcare provider is your best resource for information about what you can expect.
Self-care is an important part of living with colon cancer, but everyone’s situation is different. People treated for early-stage colon cancer may become cancer-free. They’re cancer survivors, but they may worry that their colon cancer will come back.
People who have advanced colon cancer have different concerns. They’re also cancer survivors. But for them, living with colon cancer may mean treatment that eases symptoms but doesn’t cure colon cancer. They may benefit from having palliative care. Palliative care helps people manage cancer symptoms and treatment side effects.
Follow-up colon cancer care varies depending on the cancer stage. For example, people who have surgery for Stage 0 or Stage I colon cancer may have a colonoscopy one year after surgery, another colonoscopy three years after surgery and a third five years after surgery.
Unless the follow-up colonoscopies find signs of cancer, someone with Stage 0 or Stage 1 colon cancer may be able to wait several more years before having another colonoscopy.
People successfully treated for Stage II or Stage III colon cancer will need to see their healthcare provider every three to six months for the first two years after treatment and are typically followed for five years from surgery. They may have tests including colonoscopies, CEA blood tests and imaging tests.
Anyone recovering from colon cancer treatment should contact their healthcare provider if they notice changes that may indicate the cancer has come back or is spreading.
If you’re receiving colon cancer treatment, ask your healthcare provider about symptoms that may be signs you should go to the emergency room. You may need to go to the emergency room if you have:
Most people have heard of colon cancer, which is the third most common cancer diagnosed in the U.S. If you have colon cancer, you probably want to know more about your specific situation. Here are some questions you may want to ask your healthcare provider:
A note from Cleveland Clinic
Thanks to more people taking time for colon cancer screening, healthcare providers are able to catch and treat colon cancer before it causes symptoms, much less spreads. Recent survival rate data show that more than 90% of people treated for early-stage colon cancer were alive five years after diagnosis. People with colon cancer also benefit from having newer treatments that target cancer. If you have colon cancer, ask your healthcare provider about newer treatments that may be appropriate for your situation.
Last reviewed by a Cleveland Clinic medical professional on 11/14/2022.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy