Overview

If you have Parkinson’s disease or another movement disorder, Cleveland Clinic’s Center for Neurological Restoration can help. Our center is among the first in the world to bring together an interdisciplinary team of renowned neurologists, neurosurgeons, psychiatrists, neuropsychologists, researchers, biomedical engineers, imaging specialists, physician assistants, nurses and other specialists who offer the latest medical and surgical treatments for patients with neurological and psychiatric disorders.
Movement disorders treated at Cleveland Clinic
- Parkinson’s disease
- Atypical parkinsonian disorders
- Essential tremor and other tremor disorders
- Dystonia, including torticollis and blepharospasms
- Restless legs syndrome (RLS)
- Tourette syndrome and tic disorders
- Huntington’s disease and chorea
- Ataxia
- Myoclonus
- Hemifacial spasms
- Gait disorders
Why Choose Us?
We offer you the most advanced and specialized care, complemented by leading programs in research and education. The Center for Neurological Restoration is nationally recognized for expertise in medical management and innovation in the surgical treatment of movement disorders, such as deep brain stimulation (DBS), which is an option for select patients with Parkinson’s disease, essential tremor and some forms of dystonia. Our staff are also studying how DBS may alleviate other conditions, including obsessive-compulsive disorder, Tourette syndrome, some forms of chronic pain, and weakness following stroke. We also offer other functional neurosurgical procedures such as MRI-Guided Focused Ultrasound and gamma knife surgery (for tremors), spinal cord stimulation surgery (for various pain syndromes), and shunt procedures (for normal pressure hydrocephalus).
The center has earned international recognition for setting the standards of care for movement disorders including:
- Parkinson's Foundation Center of Excellence
- CurePSP Foundation PSP Care Center
- Huntington Disease Society of America Center of Excellence
Parkinson's Disease

Parkinson’s disease is a chronic, progressive disorder that affects nerve cells (neurons) in the basal ganglia, an area of the brain responsible for coordination and fluidity of movement. These cells normally produce dopamine, a chemical that transmits signals between areas in the brain. Working properly, these signals coordinate smooth, balanced muscle movement. Parkinson’s disease, however, causes the neurons to die sooner, leading to a lack of dopamine in the brain. With this loss, patients experience more difficulty controlling their body movements.
What are the symptoms of Parkinson’s disease?
Symptoms of Parkinson’s disease vary greatly among individuals, which can make diagnosis difficult. Common symptoms include:
- Tremor or shaking that begins in a hand, leg or other body part. In some cases, tremor is confined to one side of the body. However, it may spread as the disease progresses and it can worsen with stress.
- Bradykinesia or slowness of movement may occur with dressing, bathing or other daily activities.
- Rigidity or stiffness in the limbs caused by involuntary muscle tensing, makes it difficult for a person to move freely.
- Muscle aches or pains seen mostly when medications start losing their effect.
- Balance and coordination problems usually surface as the disease progresses, and may include a forward or backward lean, or a posture in which the head is bowed and shoulders slumped.
- Other symptoms may include depression, lack of interest in activities, feelings of fear and anxiety, decreased facial expressions, difficulty swallowing and chewing, speech changes, drooling, cramped handwriting, urinary problems or constipation, sleeping problems and even skin problems, such as dandruff and greasy scalp and forehead.
Diagnosis
After a healthcare provider examines your symptoms and reviews your medical history, if they suspect Parkinson’s disease, they may recommend the following imaging and diagnostic tests:
- Blood tests (these can help rule out other forms of parkinsonism).
- Computed tomography (CT) scan.
- Genetic testing.
- Magnetic resonance imaging (MRI).
- Positron emission tomography (PET) scan.
Treatments
Treatments can vary from person to person but medications are the primary form of treatment for early disease. As the disease advances, some patients may benefit from advanced therapies such as continuous infusion pumps, MRI guided focused ultrasound and surgical options such as deep brain stimulation.
Get more details about Parkison’s disease treatment.
Parkinson’s Disease Support
EMPOWER U®: Taking Control of Parkinson’s Disease is a free, education-driven, one-day event which brings together Parkinson’s disease patients and their families and caregivers.
Care Partner U is an extension of EMPOWER U tailored for families and care partners of individuals with Parkinson’s disease.
Atypical Parkinsonian Disorders
Atypical Parkinsonian Disorders
Atypical parkinsonian disorders, or APDs, are a group of neurodegenerative conditions that present some of the most challenging diagnostic puzzles in the field of neurology, and their progressive nature can make them difficult to treat.
There are four types of atypical parkinsonian disorders:
- Progressive Supranuclear Palsy (PSP) – a condition that affects certain areas of the brain causing issues with balance, early problems with falling, eye movement, walking, thinking and swallowing.
- Multisystem atrophy or Multiple System Atrophy (MSA) – a condition that affects the central nervous system and autonomic nervous system causing issues with involuntary bodily functions.
- Dementia with Lewy Bodies (DLB) – a type of dementia that causes damage to the neurons in the brain responsible for mental capabilities, behavior, movement and sleep.
- Corticobasal Degeneration – a brain disorder that damages cells causing parts of the brain to shrink or atrophy affecting a person’s ability to talk, swallow, move and think.
What are the symptoms of Atypical Parkinsonian Disorders?
These symptoms may overlap with typical Parkinson’s disease but are seen early in the disease process and are often more severe in atypical parkinsonian disorders.
- Balance problems.
- Difficulty swallowing.
- Memory problems.
- Muscle spasms, muscle twitches (myoclonus) and muscle contractions (dystonia).
- Trouble completing tasks like using utensils or buttoning a shirt.
- Difficulty coordinating fine movements (apraxia).
- Difficulty controlling one limb (alien limb syndrome) and slowed movements (bradykinesia).
- Slurred or slow speech or difficulty finding the right words (aphasia).
- Tremors.
- Rigidity or stiffness.
- Sleep problems.
- Autonomic dysfunction or issues with the body’s ability to run processes automatically.
Treatments
Treatments can vary from person to person. Get more details about Atypical Parkinsonian disorders treatment.
Dystonia
Dystonia is a movement disorder in which forceful, sustained muscle contractions cause twisting and repetitive movements or abnormal postures. These involuntary and sometimes painful movements may affect a single muscle; a group of muscles such as those in the arms, legs or neck; or the entire body.
Dystonia causes varying degrees of disability and pain. It is a chronic disorder but, fortunately, does not usually affect cognition or intelligence. While there is no cure for dystonia, multiple treatment options can reduce the severity of symptoms.
What are the symptoms of dystonia?
Early symptoms of dystonia may include:
- Deterioration in handwriting.
- Foot cramps.
- A dragging foot after running or walking a significant distance.
Other possible symptoms include:
- Tremor.
- Headshaking.
- Involuntary blinking.
- Voice or speech difficulties.
Primary or idiopathic dystonia cases have no connection to disease or injury and many cases appear to be inherited. Dystonia also can be symptoms of other diseases, some of which may be hereditary. In some individuals, symptoms of dystonia appear in childhood. In others, symptoms may not appear until later in life.
Dystonia can be generalized (affecting most muscle groups) or focal, only affecting a few muscles in one body part. Common focal dystonias include blepharospasms (causing eyelid closure), torticollis (affecting the neck), writer’s cramp (affecting the hand and forearm during writing), and spasmodic dysphonia (affecting the vocal cords and voice).
Initially, dystonic movements are intermittent and appear only during voluntary movements or stress. Later, individuals may show dystonic postures and movements while walking or even while relaxed. Dystonic motions may lead to permanent physical deformities by causing the muscles or tendons to shorten.
Treatments
Treatments can vary from person to person. Get more details about dystonia treatment.
Essential Tremor
Many people have experienced shaky hands, especially at times of high stress or anxiety. But for 5 million Americans, involuntary shaking — or essential tremor — is a constant problem.
Essential tremor is an uncontrollable shaking of the muscles, usually upon movement. It can occur any time, but commonly begins at middle age. While the cause of essential tremor remains unknown, a family history exists in about half the cases. Essential tremor does not affect life expectancy, but it can become disabling for many common activities, such as writing and eating.
What are the symptoms of essential tremor?
Because there is less recognition of essential tremor, it is often confused with Parkinson’s disease. The difference lies in when the tremors occur. With few exceptions, in Parkinson’s disease, tremors most commonly occur when a person is at rest and diminish when there is movement. With essential tremor, shaking typically occurs with activity and diminishes at rest. The forms and circumstances where tremors are likely include:
- Action tremor: This is a form of essential tremor that happens during actions, such as reaching for an object.
- Postural tremor: This is shaking that happens when you hold part of your body in a specific pose, such as holding a hand outstretched and keeping it at the same height.
Other symptoms of essential tremor may include:
- Shaky voice.
- Nodding head.
- Balance problems.
Treatments
Treatments can vary from person to person. Get more details about essential tremor treatment.
Huntington’s Disease
Huntington's disease is a genetic condition that causes the gradual decline and death of brain cells. The disease mainly impacts regions in the brain responsible for conscious movement control and memory formation. People with Huntington's disease experience involuntary movements, cognitive decline, and shifts in both behavior and personality. These symptoms get worse as the condition progresses.
Our multidisciplinary clinic provides comprehensive care for patients and families dealing with Huntington’s disease. Our team is comprised of healthcare providers from neurology, psychiatry, neuropsychology, genetics, physical therapy, occupational therapy, and speech therapy who work in a coordinated fashion to assess the physical, emotional, cognitive, and behavioral needs of patients with Huntington’s disease. Opportunities for participation in clinical research and clinical trials are also available.
What are the symptoms of Huntington’s disease?
Huntington’s disease causes both physical and mental symptoms, including:
- Chorea - Uncontrolled movements like jerking or twitching. This usually begins in the hands, fingers and facial muscles, spreading as the disease progresses. Chorea can make everyday activities difficult to perform.
- Ataxia - Loss of coordination.
- Trouble walking.
- Dysphagia - Difficulty swallowing.
- Slurred speech.
- Emotional changes like mood swings, depression and irritability.
- Problems with memory, focus and multitasking.
- Trouble learning new information.
- Difficulty making decisions and reasoning.
Treatments
Treatments can vary from person to person. Get more details about Huntington’s disease treatment.
Functional Movement Disorders
Functional Movement Disorders or FMD, makes your body move in ways you can't control like shaking, repeated actions, or sudden muscle movements. Unlike conditions like Parkinson's disease, FMD happens because of a problem with how your brain handles movement control. Even though your brain is creating these movements, they feel completely out of your control.
Individuals with FMD aren't pretending or making up their symptoms. They can't just stop the movements by trying harder or thinking differently. In fact, when people focus on their movements, they often get worse. The movements usually get better when the person is distracted.
What are the symptoms of Functional Movement Disorders?
The symptoms of FMD are abnormal, uncontrollable movements. Examples include:
- Tremor, or shakiness in your limbs.
- Dystonia: Uncontrollable muscle movements, which can result in repetitive or twisting movements.
- Jerks or myoclonus: Abnormal sudden and brief muscle movements.
- Gait and balance issues.
- Limb weakness.
Diagnosis
Your provider will review your symptoms and medical history followed by a physical and neurological exam. The main way to diagnose FMD is understanding what makes a patient’s abnormal movements worse. Your provider may also recommend neuropsychological testing.
Treatment
FMD symptoms aren’t caused by permanent brain damage, meaning its possible to make a full recovery. Treatment includes:
- Fully understanding FMD diagnosis.
- Readiness for symptom improvement.
- Sticking to your treatment plan.
A combination of therapies are often recommended. These treatments may include:
Diagnosis and Treatments
Movement disorders affect people differently from the parts of the body impacted to the symptoms you experience. Our providers will begin with a physical exam and a neurological exam. Then, they may order additional tests to rule out other conditions, like:
- Blood tests
- Electromyography (EMG)
- Electroencephalogram (EEG)
- Spinal tap (lumbar puncture)
- Nerve conduction study
- Neuropsychological testing
- Skin Biopsy
You may also have imaging tests like a CT scan or MRI so our team can look closely at your nerves, brain, and spinal cord. Additionally, a nuclear medicine study called Dopamine Transporter SPECT Scan may sometimes be ordered to differentiate Parkinson’s disease from other causes of tremor.
Movement disorders affect everything from the way you write to how you walk, talk and swallow. It depends on the kind of movement disorder you have and how badly it affects you. That’s why we craft your treatment plan based on your specific diagnosis and needs.
We may manage your condition with:
Medical Options
Medical management is the cornerstone of movement disorder care. Pharmacological management (such as oral medications and botulinum toxin injections), patient education and family support are essential aspects of the comprehensive treatment plan we provide for each of our patients. As movement disorders are often accompanied by “non-motor” complications, our team includes specialists with different areas of expertise who can use a variety of treatment approaches to address mood disorders, memory or cognitive disorders, sleep disorders and autonomic (blood pressure, bladder, swallowing) disorders. Our comprehensive approach to care optimizes treatment of all these related symptoms to improve quality of life.
Advanced Therapies and Surgical Treatment
Cleveland Clinic Center for Neurological Restoration offers the latest surgical and non-surgical treatment options for movement disorders that can be customized to achieve patient-driven goals. Our team ranks among the world’s leaders in deep brain stimulation (DBS) surgery and has performed thousands of DBS surgeries for Parkinson’s disease, essential tremor and some forms of dystonia. Our broad portfolio of options also includes incisionless procedures, such as high-intensity focused ultrasound (HIFU) and Gamma Knife® radiosurgery, allowing us to find successful treatment options for many patients with different goals or clinical needs.
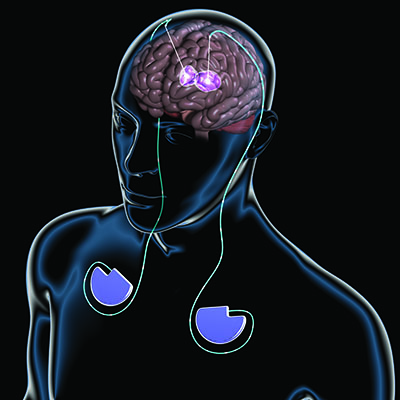
Deep Brain Stimulation (DBS)
DBS involves implanting a device in the brain that sends mild electrical impulses to parts of the brain where faulty electrical signals trigger abnormal movement symptoms.
DBS successfully treats young as well as some elderly patients, provided their health is otherwise good. However, it is not for everybody. Generally, DBS candidates are patients who:
- Have a declining quality of life due to functional impairment related to a movement disorder.
- Are experiencing a worsening of coordination and control of movement.
- Have had an adequate trial of medications.
- Are not impaired by dementia, uncontrolled depression, or anxiety.
- Do not have severe medical comorbidities that make elective surgeries risky.
A successful outcome depends as much on selecting the right patient as on having a skilled surgical team. That’s why DBS candidates first undergo an evaluation by several specialists, including a neurologist, neurosurgeon, psychologist, and neuropsychologist with special training in DBS.
Advanced brain imaging and computer technology are used to pinpoint the areas of the brain causing symptoms. Guided by this information, a neurosurgeon makes a small opening in the skull and implants electrodes in targeted areas of the brain. Depending on the patient’s needs, this procedure is done on one or both sides of the brain.
The patient usually goes home one or two days following surgery and returns to the hospital one week later for a second step. The surgeon now implants a “brain pacemaker (a battery-powered pulse generator) under the patient’s collarbone, which is linked to the electrodes implanted earlier in the brain. The pulse generator delivers stimulation to these targeted brain areas, blocking the abnormal signals that produce symptoms.
The patient goes home in less than 24 hours and returns as an outpatient two to four weeks later to turn on and program the pulse generator. Several visits might be necessary to fine-tune the device to control an individual’s particular symptoms. It can often be adjusted over time to accommodate changes in the underlying disorder. This process is painless. At home, the patient can switch the stimulation on or off or even control settings between different options the clinician has found to be well tolerated and potentially effective in the office. The device’s batteries generally last three to five years. However, there are also rechargeable batteries that last about 15 years.
For those patients who cannot tolerate or are not considered candidates for traditional DBS surgery, Cleveland Clinic pioneered the use of an interventional MRI suite attached to a conventional operating room, called IMRIS Neuro, to plan and precisely place the leads while the patient is under general anesthesia. Before this invention, almost all DBS required awake surgery, but this advancement offers patients the option of being asleep during the implant surgery.
Are there risks involved with DBS?
As with any surgery, the DBS procedure is not risk-free. There is a risk of brain hemorrhage or stroke that may result in neurological impairments such as paralysis, speech impairment, mental impairment, or other neurological problems. Other risks include infection, need for additional surgery, pain, and anesthesia-related complications. While there is always a risk of death in brain surgery, this is not common. Most patients will complete the surgery without significant complications.
DBS Second Opinion Program
Our DBS specialists offer second-opinion consultations to patients who underwent DBS surgery outside of Cleveland Clinic and are not experiencing optimal results. Our multidisciplinary team is skilled at troubleshooting complex cases. They will review and evaluate your imaging and test records to determine the best course of action, which may involve DBS programming, medication correction, or lead placement adjustment surgery.
High-Intensity Focused Ultrasound (HIFU)
HIFU is a minimally invasive procedure that uses heat created by concentrated ultrasound waves to block signals in the brain that cause tremor.
Experts can use HIFU to treat tremors on one side of the body, and sometimes, patients may benefit from having the other side treated later as well. Generally, HIFU may be an option for patients with:
- A confirmed diagnosis of essential tremor or tremor-dominant Parkinson’s disease.
- Tremors that have not been relieved by medications.
- Tremors that limit your ability to perform daily activities.
A successful outcome depends as much on selecting the right patient as on having a skilled surgical team. That’s why HIFU candidates first undergo an evaluation by several specialists, including a neurologist, neurosurgeon, neuroradiologist, and neuropsychologist with extensive training in HIFU techniques.
The surgical team uses MRI to precisely identify the part of the brain that will be treated and position the ultrasound device that sends high-frequency sound waves to the targets in the brain. They start the procedure with low-energy pulses to be sure the targeted location is getting treatment. Once they confirm the tremor is improving, they will raise the temperature of the ultrasound waves to deliver a full dose.
HIFU treatment typically takes between two and four hours. The patient may be lightly sedated but will remain awake throughout the procedure so that the surgical team can confirm the tremor is getting better in real-time. After the procedure, patients can return home.
Are there risks involved with HIFU?
As with any surgery, HIFU is not risk-free. Most patients will complete the surgery without significant complications. In some cases, HIFU can cause temporary side effects, such as nausea, headache during the procedure, mild-to-moderate numbing and tingling in fingertips or lips, unsteadiness in walking or balance problems, and speech or swallowing problems.
Gamma Knife® Radiosurgery
Gamma Knife® radiosurgery is a minimally invasive procedure that uses radiation beams to block signals in the brain that are causing tremors. The procedure does not involve an incision.
Generally, Gamma Knife may be an option for patients with:
- Confirmed diagnosis of essential tremor or tremor-dominant Parkinson’s disease.
- Tremors that cannot be relieved by medications or deep brain stimulation.
- Tremors that limit your ability to perform daily activities.
A successful outcome depends as much on selecting the right patient as on having a skilled surgical team. That’s why Gamma Knife candidates first undergo an evaluation by several specialists, including a neurologist, neurosurgeon, and physicist with special training on the Gamma Knife procedure.
Advanced computer technology and imaging tests are used to pinpoint the areas of the brain causing tremor symptoms. They then use a Gamma Knife machine to deliver radiation beams to the target areas, sparing nearby, healthy brain tissue. Treatment usually takes one to two hours, and the patient can go home the same day.
Are there risks involved in Gamma Knife?
As with any surgery, the Gamma Knife procedure is not risk-free. There is a risk of brain hemorrhage, swelling of the brain, and seizures. Other side effects include headache, nausea and vomiting, and numbness or tingling on the scalp. Most patients will complete the surgery without significant complications.
Clinical Trials & Research
Access to Clinical Trials
Clinical trials are one of the cornerstones to advances in therapy. The most cutting-edge and promising therapies for movement disorders are tested in a safe, comfortable and ethical manner.
Patients have the opportunity to participate in these advancements and to participate in new therapies before they become commercially available. The Center for Neurological Restoration has accelerated its research activities, and now offers more than two dozen clinical trials to patients with movement disorders. A clinical trial consortium links our Cleveland, Florida and Nevada sites to ensure that patients have access to clinical trials regardless of where they are treated.
Research
Cleveland Clinic continues to conduct groundbreaking research in neurorestorative therapies for patients with disabilities secondary to neurological and psychiatric disorders, including the development of DBS to treat obsessive-compulsive disorders, depression and other neuropsychiatric disorders.
Appointment & Locations
Make an Appointment
To schedule an appointment with a movement disorders specialist in:
- Cleveland, Ohio - 866.588.2264
- Weston, Florida - 877.463.2010
- Las Vegas, Nevada - 702.483.6000
- Schedule an Appointment Online
Virtual Visits
Whether you're a new or existing patient, you can get an initial evaluation or follow-up care from a movement disorders specialist using your phone, tablet or computer. This means there's no travel or parking, less waiting and significant time savings. Call 216.636.5860 to schedule a virtual visit for you or a loved one and get details on cost and set-up instructions.
Shared Medical Appointment: Taking Control of Parkinson's Disease
Cleveland Clinic’s Center for Neurological Restoration offers patients diagnosed with Parkinson’s disease a shared medical appointment (SMA), or group sessions with fellow Parkinson’s disease patients and a healthcare professional.
The unique, eight-hour appointment offers the benefit of more time with a healthcare professional, less time spent in the waiting room, and the ability to learn from others with the same or similar conditions. Because people have different questions, many patients leave the SMA with more information than they might have gathered in a one-on-one meeting with their own physician. These appointments do not take the place of the initial personal evaluation with your neurologist.
For more information on SMAs, please call the Center for Neurological Restoration in Cleveland, Ohio at 216.445.1108.